Image Citation: [1]
Written by Maggie Ruan ‘28
Edited by Cavin Xue ‘28
Cancer – everyone knows about the heart-dropping diagnosis. Every year, millions of people are given the agonizing near-death sentence [2]. Yet, even after centuries, we’ve made little progress in preventing or curing such an elusive disease. Despite great strides in diagnostic imaging and chemotherapy, one question remains: how much do we know about the actual mechanisms that allow cancer cells to persist against our resilient immune systems?
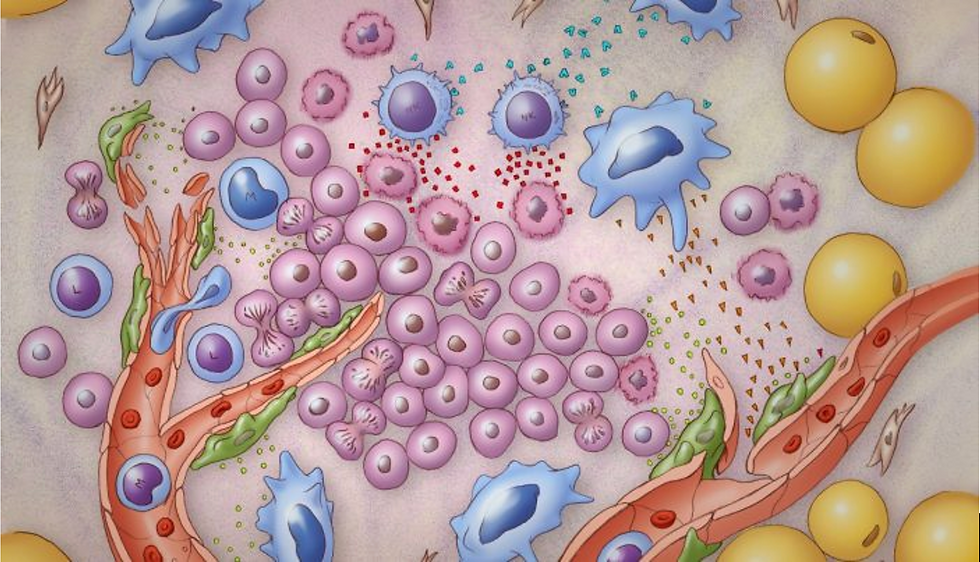
The answer lies within the tumor microenvironment, comprised of tumor cells, surrounding immune cells, blood vessels, and other molecules in our bodies. One of these immune cells, the macrophage, is the primary focus of recent cancer research.
What are Macrophages?
Macrophages are a type of immune cell that you might categorize as the “well-rounded student.” With the primary goal of engulfing and destroying foreign cells, you can find macrophages in extracurriculars such as clean-up duty, organizing efforts from other immune cells, and staying on the lookout for any pesky disruptions to your body’s immune system [2]. With their unique ability, the assumption is that macrophages play a role in eating tumor cells. Yet upon further inspection, this isn’t always the case.
Take mesothelioma, a rare cancer of the mesothelial lining (the lining of your internal organs) primarily associated with asbestos. Although less than 1% of individuals diagnosed with cancer have mesothelioma, it proves to be a deadly disease with no specific cure [4]. Asbestos is a group of fibrous minerals once used for insulation and now classified as an environmental carcinogen. Historically, mesothelioma mainly ailed construction and cargo fleet workers who were repeatedly exposed to asbestos over many years. In mesothelioma, asbestos fibers are inhaled or otherwise taken in by the body, and the inability to excrete the invaders perpetuates chronic inflammation, leading to cell malfunctions.
In mesothelioma cases, macrophages are often involved in both the tumor microenvironment and granulomatous regions (inflammation surrounding asbestos fibers). Strangely enough, the types and quantities of macrophages involved in these two regions are significantly different.
M1 and M2 Macrophages
Near the asbestos-induced inflammation, M1 macrophages dominate. M1 macrophages are widely referred to as pro-inflammatory macrophages—they play a major role in inflammation as the macrophages try to digest asbestos fibers. Unfortunately, due to the nature of asbestos, the body cannot absorb the fibers they see as invaders, causing long-term inflammation and subsequent tumor development.
Interestingly, the primary macrophage that involves itself in the actual tumor microenvironment is the M2 macrophage, which has tumor-supporting properties. Generally, M2 macrophages are known to be anti-inflammatory and tissue-repairing, which are good things – just not when it comes to cancer. M2 macrophages help build blood vessels to feed the tumor (a process called angiogenesis), suppress immune responses, and facilitate metastasis, allowing the cancer to spread. This contrast of macrophages—one type that fights tumors and another that tends to them— emphasizes the conflicting nature of the tumor microenvironment and draws attention to why targeting macrophages has become a key focus in cancer research.

Figure A shows the staining of various immune cells within the tumor microenvironment. Figure B highlights the difference in the amount and strength of staining for M1 and M2 macrophages [5].
In many types of cancers, including mesothelioma, the shift from an M1-dominant environment to an M2-dominant one is linked to a worse prognosis for patients.
Looking Toward the Future
A deeper understanding of how macrophages behave in a tumor microenvironment could revolutionize cancer therapies. A 2024 study describes “[tumor associated macrophages]-targeted therapies can be directed to drive [tumor associated macrophages] towards M-1 like macrophages, eliminate existing [tumor associated macrophages], or prevent the recruitment” of other tumor supporting cells [6].
References
[1] Murfin K. 3 things to know about the tumor microenvironment [Internet]. MD Anderson Cancer Center. 2021. Available from: https://www.mdanderson.org/cancerwise/what-is-the-tumor-microenvironment-3-things-to-know.h00-159460056.html
[2] Cancer Statistics [Internet]. National Cancer Institute. 2015. Available from: http://www.cancer.gov/about-cancer/understanding/statistics
[3] Lendeckel U, Venz S, Wolke C. Macrophages: Shapes and Functions. ChemTexts [Internet]. 2022 Mar 10;8(2). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8907910/
[4] Jain SV, Wallen JM. Malignant Mesothelioma [Internet]. Nih.gov. StatPearls Publishing; 2023 [cited 2024 Oct 22]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK519530/#article-25030.s14.
[5] Yuwaraj Kadariya, Sementino E, Ruan M, Cheung M, Parham Hadikhani, Osmanbeyoglu HU, et al. Low Exposures to Amphibole or Serpentine Asbestos in Germline Bap1-mutant Mice Induce Mesothelioma Characterized by an Immunosuppressive Tumor Microenvironment. Cancer Research Communications [Internet]. 2024 Apr 8 [cited 2024 Oct 22];4(4):1004–15. Available from: https://pubmed.ncbi.nlm.nih.gov/38592450/
[6] Zhang W, Wang M, Ji C, Liu X, Gu B, Dong T. Macrophage polarization in the tumor microenvironment: Emerging roles and therapeutic potentials. Biomedicine & Pharmacotherapy [Internet]. 2024 Jun 14 [cited 2024 Oct 6];177:116930–0. Available from: https://www.sciencedirect.com/science/article/pii/S075333222400814X#bib53

Comentarios